
Services
Prenatal care visits and childbirth.
Gynaecological endoscopy
Gynaecological endoscopy is a surgical discipline which uses optical instruments specially designed to help diagnose the most frequent female disorders and pathologies such as some infertility problems, small vaginal hemorrhages or endometrial polyps among others. Gynaecological endoscopy employs hysteroscopy and laparoscopy for these purposes.
Gynaecological endoscopy as we know it is nowadays possible thanks to important technical advances, along with the sophistication and the miniaturization of the equipment used. Modern anaesthetic medicine has also been important for the development of surgical procedures. This medicine is extremely effective, wears off quickly and its side effects have been reduced so that it can be used effectively in ambulatory surgery. Among other advances this made possible the so called minimally invasive surgery which owes its name to the fact that very small incisions are made and the intervention is ambulatory.


Gynecologic Laparoscopy
Gynecologic laparoscopy is an alternative to open surgery. It uses a laparoscope to look inside your pelvic area. Open surgery often requires a large incision.
A laparoscope is a slender, lighted telescope. It allows a doctor to see inside your body. Diagnostic laparoscopy can determine whether you have conditions such as endometriosis or fibroids. It can also be a form of treatment. With miniaturized instruments, your doctor can perform a variety of surgeries. These include:
ovarian cyst removal
tubal ligation (surgical contraception)
hysterectomy
Laparoscopy generally has a shorter healing time than open surgery. It also leaves smaller scars. A gynecologist, general surgeon, or other specialist may perform this procedure.
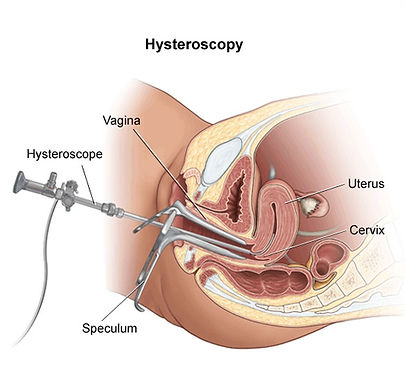
Hysteroscopy
Hysteroscopy is the visual examination of the canal of the cervix and interior of the uterus using a thin, lighted, flexible tube called a hysteroscope. The device is inserted through the vagina.
Hysteroscopy may be used for both diagnostic and therapeutic purposes. The hysteroscope allows for easy visual access to the interior of the cervix and uterus to assess the lining of these structures. Therapeutic maneuvers, such as taking a tissue sample (biopsy), removal of polyps or fibroid tumors, or preventing bleeding with cautery (destruction of tissue by electric current, freezing, heat, or chemicals) may be performed during a hysteroscopy procedure.
Diagnostic hysteroscopy may be performed in a doctor's office with local or no anesthesia required. More invasive therapeutic hysteroscopy procedures may be performed in the operating room under local, regional, or general anesthesia.
Because the doctor is able to see the interior of the cervix and uterus during the procedure, diagnostic hysteroscopy has become a more common procedure than dilation and curettage (D & C), which is performed without endoscopic visualization.
Other related procedures that may be used to evaluate problems of the female pelvic organs include D & C, cervical biopsy, colposcopy, endometrial biopsy, laparoscopy, Pap test, and pelvic ultrasound.
Infertility
Infertility is defined by the American Society for Reproductive Medicine (ASRM) as a disease of the reproductive system that impairs the body's ability to perform the basic function of reproduction. Although conceiving a child may seem to be simple and natural, the physiological process is quite complicated and depends on the proper function of many factors, including the following, as listed by the ASRM:
Production of healthy sperm by the man
Production of healthy eggs by the woman
Unblocked fallopian tubes that allow the sperm to reach the egg
The sperm's ability to fertilize the egg
The ability of the fertilized egg to become implanted in the uterus
Adequate embryo quality
Who is affected by infertility?
Infertility affects about 12 percent of couples of childbearing age. Infertility is not just a woman's concern. A problem with the male is the sole cause, or a contributing cause, of infertility in about 50 percent of infertile couples. About one-third of infertile couples have more than one cause or factor related to their inability to conceive.
What causes infertility?
Many different factors and problems can cause infertility, including problems in the female reproductive system, the male reproductive system, or a combination of the two. The following are some of the conditions or factors that are associated with infertility:
Female factors
Ovulation dysfunction. With this condition, the woman's reproductive system does not produce the proper amounts of hormones necessary to develop, mature, and release a healthy egg.
Anatomical problems. Abnormal development or function of the female anatomy can prevent the egg and the sperm from meeting. The most common anatomical problem is blockage of the fallopian tubes. Other anatomical problems may include the presence of pelvic scar tissue from previous surgeries or infections.
Endometriosis. Endometriosis is a condition in which the tissue that lines the uterus develops outside the uterus, usually on other reproductive organs inside the pelvis or in the abdominal cavity. Each month, this misplaced tissue responds to the hormonal changes of the menstrual cycle by building up and breaking down, resulting in internal bleeding which can cause scar tissue to form and affect reproductive organ function.
Birth defects. Abnormal development and function of reproductive organs resulting from birth defects can affect fertility. One of the most common reproductive system birth defects occurs following a woman's exposure to DES (diethylstilbestrol) taken by her mother during pregnancy. In years past, DES was given to women at risk for pregnancy loss. Fetal DES exposure often causes abnormal development of the uterus and cervix.
Infection. Pelvic inflammatory disease (PID) is caused by a type of bacteria such as gonorrhea and chlamydia. PID can affect the uterus, fallopian tubes, and/or the ovaries. It can lead to pelvic adhesions and scar tissue that develops between internal organs, causing ongoing pelvic pain and the possibility of an ectopic pregnancy (the fertilized egg becomes implanted outside the uterus).
Immunological problems. A problem with a woman's immune system can lead to pregnancy loss. Antibodies (immune or protective proteins) in a woman's system can fail to recognize a pregnancy, or there may be an abnormal immune response to the pregnancy. Women can also develop antisperm antibodies which attack and destroy sperm.
Male factors
Low or absent sperm production. Without proper numbers of healthy sperm, the chance of fertilization is decreased.
Abnormal sperm function. Sperm must have proper motility and the ability to penetrate the egg.
Varicocele. This is a condition in which varicose veins develop around the testes. It is a very common cause of male factor infertility and is usually treatable and reversible with surgery.
Lifestyle. Use of recreational drugs (i.e., marijuana, cocaine), heavy alcohol use, cigarette smoking, certain medications, and excessive heat to the genital area (as in hot tubs) can affect sperm quality and function.
Hormonal disorders. Improper male hormone or endocrine function can affect sperm production and fertilization ability.
Chromosomal defects. Certain chromosomal abnormalities are associated with male infertility.
Birth defects. Abnormalities in a man's reproductive system can occur during fetal development. Some birth defects are due to a man's exposure to DES (diethylstilbestrol) taken by his mother during pregnancy.
Immunological problems. A man may have antisperm antibodies (immune or protective proteins) which attack and destroy sperm
How is infertility diagnosed?
When conception does not occur after one year of unprotected intercourse, after six months in women over age 35, or if there are known problems causing infertility, a medical evaluation of both the male and female is recommended. Some obstetrician/gynecologists (OB/GYNs), certified nurse midwifes (CNMs), and nurse practitioners (NPs) are able to provide basic infertility evaluation and treatment. However, many causes of infertility are best treated by a board-certified reproductive endocrinologist. This is an OB/GYN who has had additional education and training in infertility and is certified with the American Board of Obstetrics and Gynecology in the sub-specialty of Reproductive Endocrinology and Infertility.
Generally, the OB/GYN or reproductive endocrinologist will evaluate specific situations and perform tests in both the male and female partners to determine the cause of infertility. The doctor is looking for answers to the following questions:
Is the female ovulating regularly?
Is the male producing healthy, viable sperm?
Are the female's egg and the male's sperm able to unite and grow normally?
Are there any obstacles to proper implantation and maintenance of the pregnancy?
The following tests are often part of the basic medical workup for infertility.
Both partners
Medical and sexual history (to evaluate possible physical causes of infertility and if sexual intercourse has been appropriately timed)
Female
Physical examination. A complete physical examination (including a Pap smear and testing for infection) will be necessary.
Ovulation evaluation. An evaluation of ovulation function using an analysis of body temperatures and ovulation called the basal body temperature chart, or with ovulation prediction methods using urine samples, may be recommended.
Hormone testing. Hormone testing may be recommended, as certain hormones increase and decrease in production at various times in the monthly cycle.
Ultrasound. Ultrasound can show the presence of follicles (the sacs containing developing eggs) and the thickness of the uterine tissues. Ultrasound can also show abnormal conditions, such as ovarian cysts or fibroids (benign tumors in the uterus).
X-rays. A hysterosalpingogram may be recommended. This test uses a radio-opaque dye injected into the cervical opening to visualize the inside of the uterus and determine if the fallopian tubes are open.
Male
Semen analysis. A collection of a semen sample obtained by masturbation that is analyzed in the laboratory for the sperm count, sperm motility, sperm shape, quantity, and evaluation of the ejaculate liquid may be recommended.
Other tests may be performed that evaluate the sperm's ability to penetrate the egg, as well as male hormone testing.
Men may be referred to a urologist for further evaluation.
To Schedule An Appointment
Call 24625880
Colposcopy
Colposcopy is a procedure that uses an instrument with a magnifying lens and a light, called a colposcope, to examine the cervix (opening to the uterus) and vagina for abnormalities. The colposcope magnifies the image many times, thus allowing the health care provider to see the tissues on the cervix and vaginal walls more clearly. In some cases, a cervical biopsy, a small sample of tissue, may be taken for further examination in the lab.
Reasons for the procedure
When cervical or vaginal problems are found during a pelvic examination, or abnormal cells are found during a Pap test, a colposcopy may be performed. Through the colposcope, the health care provider can see certain changes in cervical and vaginal tissues, such as abnormal blood vessels, tissue structure, color, and patterns. Cells that appear to be abnormal, but are not cancerous at the present time, may be identified as precancerous. The appearance of these abnormal cells may be the first evidence of cancer that develops years later.
If abnormal tissue is seen during a colposcopy, a small sample of tissue (called a colposcopic biopsy) may be taken for further study. The health care provider may also take tissue samples from inside the cervix using an endocervical brush or endocervical curettage (ECC).
A colposcopy procedure may also be used to diagnose and assist in the treatment of the following conditions:
· Bleeding
· Polyps (benign growths)
· Genital warts, which may indicate infection with human papilloma virus (HPV), a risk factor for developing cervical cancer
· Diethylstilbestrol (DES) exposure in women whose mothers took DES during pregnancy, as DES exposure increases the risk for cancer of the reproductive system
There may be other reasons for your health care provider to recommend colposcopy.
DR. GEORGE LEONTIADES
Apollonos 3, 6016 Larnaca,Cyprus.
Tel 24625880
Fax 24665751
ΔΡ. ΓΙΩΡΓΟΣ ΛΕΟΝΤΙΑΔΗΣ
Απόλλωνος 3, 6016 Λάρνακα, Κύπρος.
Τηλ 24625880
Φαξ 24665751




